The MPS Society has been funding cutting-edge research into MPS, Fabry and related diseases since its inception in 1982.
To this day, the MPS Society has spent over £12 million on research projects into these conditions, to find better treatments and care. Scientific breakthroughs and new technologies offer hope for diagnoses and treatments for those affected that was unimaginable a few years ago.
The sooner we can accelerate our research and take advantage of these opportunities, the quicker we can help even more people affected by MPS, Fabry or a related lysosomal disease.
Grants for research into psychological wellbeing and newborn screening
We are inviting grants for scientific or clinical research with a particular focus on newborn screening or that support and/or improve the psychological wellbeing of those impacted by LSD or related conditions.
Clinical Scientific Advisory Board (CSAC)
Our Clinical Scientific Advisory Committee (CSAC) consists of members of our Board of Trustees and the Society’s Patient Advocacy team. These members come from medical, healthcare or research backgrounds from a broad range of disciplines and perspectives who will consider research applications each year.
All proposals will be subject to a review process to ensure they meet our high standard of quality. The committee will make an informed recommendation to our Board of Trustees who hold the final decision on how we allocate research funds.
Applications for grants will be assessed on:
The importance or burden of the health or care problem being studied
What the proposed research adds to the existing body of knowledge
The improvements in health and care this research is likely to lead to
The potential impact of the research on patients, the public and people working in health and care
Whether the cost of the research is reasonable and commensurate with the work involved
The likelihood that the research design is feasible and deliverable and answers the proposed question
We will consider applications across the breadth of metabolic medicine, but of course, will focus on MPS and related disorders.
Conflicts of interest
Both the Clinical and Scientific Advisory Committee and any external reviewers are asked to declare any conflicts of interest. Those with conflicts are not permitted to discuss or provide comment on those applications.
Relevant research
Rare Disease Research Partners
RDRP support research and access to treatment for people living with rare conditions.
Funded research
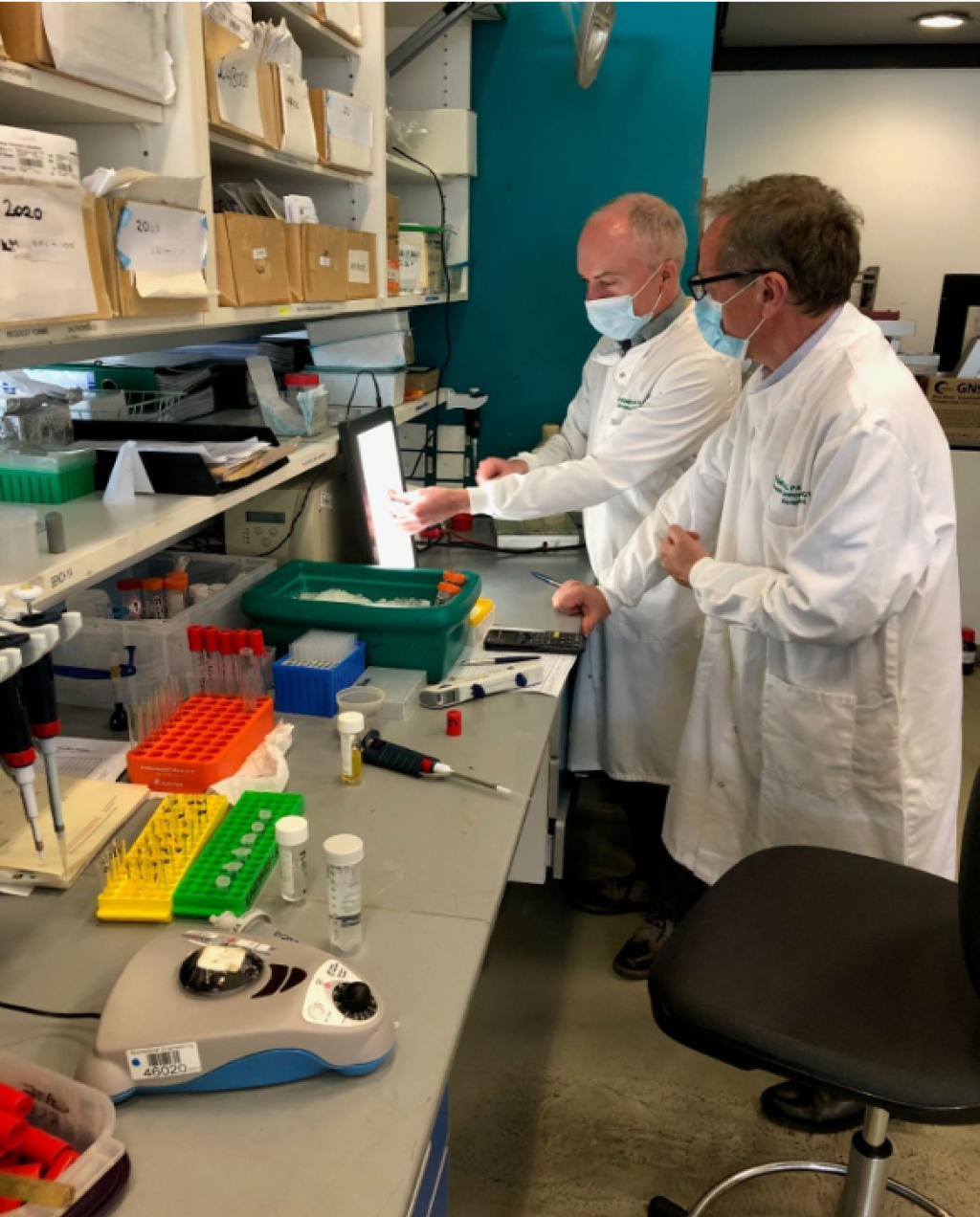
In January 2020, the MPS Society awarded a grant to Professor Simon Heales of Great Ormond Street Hospital, London to employ a scientist for one year to evaluate a new piece of equipment that could significantly improve our ability to identify patients with lysosomal disorders such a MPS I, Pompe, Fabry and Gaucher Disease.
Research grant application process
Applications for research grants are now open until 28 March
The MPS Society is open to applications for grants for scientific or clinical research into LSD or related conditions from Monday 8 January 2024. The deadline for applications is 28 March 2024. Following a review of its patient support, in this round of grants we are particularly interested in receiving applications that support and/or improve the psychological wellbeing of those impacted by LSD or related conditions or have a focus on newborn screening. While the MPS Society will accept applications from single centres or research units, we are specifically looking for applications from applicants collaborating with other centres or units in the field.
Can you join the peer review panel?
We are committed to transparency and open access and applications will be sent out for peer-review. We would encourage all applicants, potential applicants or people with an interest to help us support impactful research by joining our peer review panel, if you are willing to spare a couple of hours reviewing an application please contact the peer review coordinator.
Application FAQs
Applications for research grants are now open until Thursday 28 March 2024 and will be reviewed at one of the peer review committee meetings throughout the year. Download and complete our grant application form now.
Following submission, grant applications will be reviewed internally by members of the MPS Society’s Clinical and Scientific Advisory Committee (CSAC). This committee includes trustees with a medical or scientific background, non-medical trustees and members of the MPS Society’s Support and Advocacy senior team. A shortlist of applications will then be sent for external peer review, by a panel of relevant medical experts. It should be noted these may include international experts.
We are committed to transparency and open access and applications will be sent out for peer-review.
All applicants, successful or otherwise, will receive anonymised feedback from the Clinical and Scientific Advisory Committee and where available the peer review panel.
Detailed Terms and Conditions of Medical Research Grants, the MPS Society’s Moral and Ethical Policy for Fundraising and Public Affairs Activities and acceptance forms are attached with the application form.
Research grant payments will be made quarterly in arrears. Quarterly payments beyond the first quarter for second and third year grants will only be made after a review of the research project has been undertaken and an appraisal report received.
A final report must be submitted within two months of the end of the research grant and include:
A summary of the results of the research project
Indication of whether goals were met
If applicable suggestions for further research efforts needed in the field
A summary statement in lay language of the results of the research which will be communicated via emails and social media.
If the results are published in any scientific journals, provision of a copy of the article(s) is required.
The MPS Society requests that all acknowledgements include the following: ‘This work was supported by a research grant from the Society for Mucopolysaccharide Diseases (MPS Society) www.mpssociety.org.uk’
When you submit the application you will need to include:
CV of lead investigator
Detailed budget