In the course of normal life there is a continuous recycling process, this process requires a series of biochemical tools called enzymes. People with MLD lack a specific enzyme called arylsulphatase A which breaks down sulphatides, or the protein saposin B which works with arylsulphatase A to break down sulphatides. When arylsulphatase A and saposin B are unable to work together to break down sulphatides, they build up in cells within the nervous system, including the brain.
Metachromatic leukodystrophy (MLD) is an inherited lysosomal storage disease that progressively destroys nerve cells (neurons) in the brain and spinal cord.
Read on for information about the condition or see the latest updates and resources.
Frequently asked questions
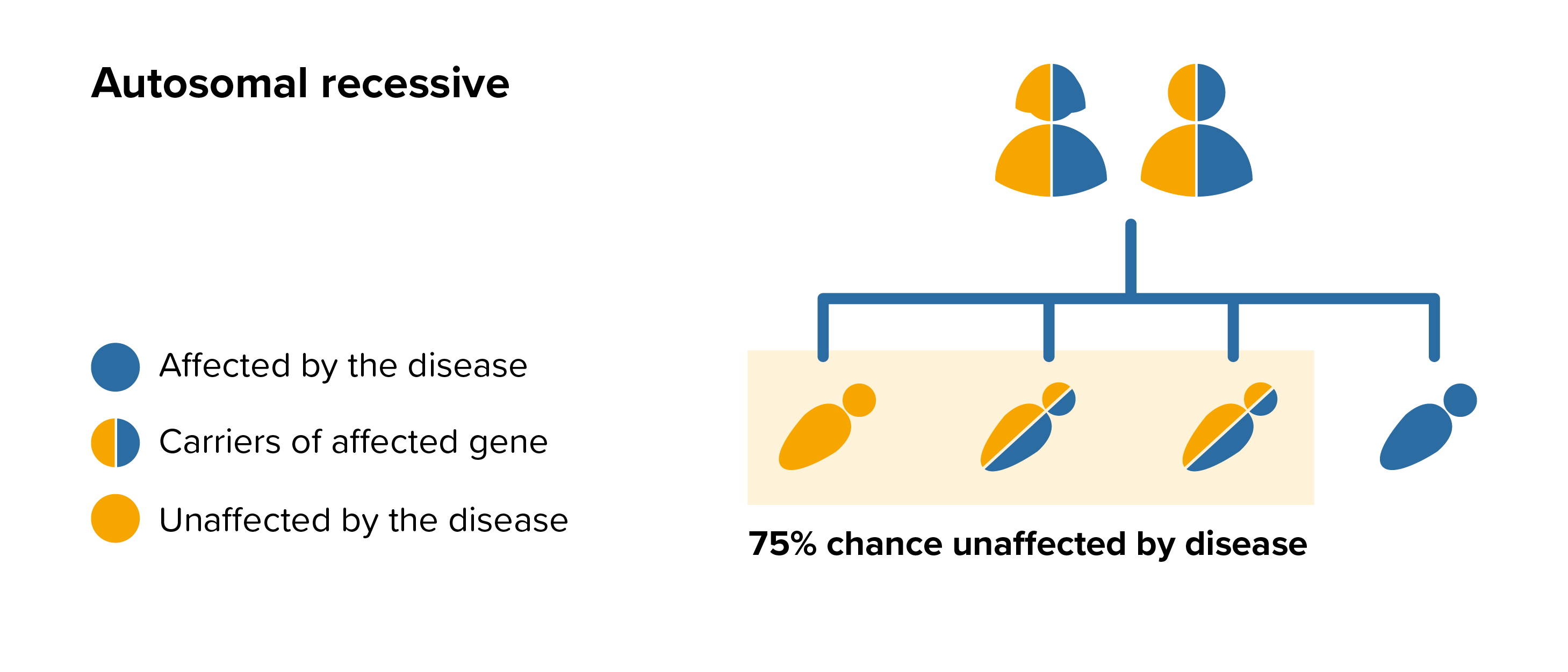
MLD is an autosomal recessive disease this means that both parents must carry the same affected gene and each pass this same affected gene to their child.
People probably carry from 5 to 10 genes with mutations in each of their cells. Problems happen when the particular gene is dominant or when a mutation is present in both copies of a recessive gene pair. Genes are the unique set of instructions inside our bodies that make each of us an individual. They are the blueprint for our growth and development, as well as controlling how our bodies function.
Genes are carried on structures called chromosomes and it is usual to have 23 pairs. A child will inherit half of the chromosomes from the mother and the other half from the father resulting in 23 pairs. 22 of these pairs look the same in both males and females. Pair 23 are the sex chromosomes, and this is the pair that differ between females and males. The X chromosome is inherited from the mother and the Y chromosome is inherited from the father. More information about inheritance is available in our publication.
For each pregnancy the chances of a baby inheriting MLD are completely independent of whether a previous child was affected with MLD. With each pregnancy there is a 1 in 4 chance that the baby will be affected by MLD.
 All parents of children with MLD can benefit from genetic counselling, the counsellor can provide advice on the risk to close relatives and to suggest whether the wider family should be informed. To find out during a pregnancy, if the baby is affected by MLD, screening tests can be arranged early on during a pregnancy for those families who already have a child with MLD. Where only one parent is a carrier, they can opt for carrier screening but it is not 100% reliable or accurate and is not possible in all cases. Amniocentesis and chorionic villus sampling are both available during the pregnancy to find out if the baby is affected by MLD.
All parents of children with MLD can benefit from genetic counselling, the counsellor can provide advice on the risk to close relatives and to suggest whether the wider family should be informed. To find out during a pregnancy, if the baby is affected by MLD, screening tests can be arranged early on during a pregnancy for those families who already have a child with MLD. Where only one parent is a carrier, they can opt for carrier screening but it is not 100% reliable or accurate and is not possible in all cases. Amniocentesis and chorionic villus sampling are both available during the pregnancy to find out if the baby is affected by MLD.
It might also be possible to have Pre-implantation genetic diagnosis (PGD) screening to avoid passing MLD to the baby. PGD is an assisted fertility treatment that involves checking the chromosomes of embryos before they are transferred in the womb using IVF techniques.
It is estimated that nearly 6% of the UK population (around 3.5million people) will be affected by a rare disease at some point in their lives. A single rare disease may affect up to about 30,000 people however the vast majority of rare diseases affect far fewer than this.
MLD is the commonest of all the leukodystrophies. However, it is still a rare disease that affects between about 1 in 40,000 to 160,000 new-borns.
People with MLD can experience some or many symptoms from a wide spectrum which range from severe to very mild. The severity of MLD varies widely across 3 forms which are defined by the age of the patient when the first signs and symptoms start to appear.
Late infantile - symptoms develop between 6 months and 4 years of age.
Juvenile - symptoms first develop between 4 to 16 years of age.
Adult - symptoms develops in people 16 years and over.
Symptoms experienced in MLD vary between people, these include:
Developmental delay with significant reduction in physical, cognitive, behavioural, emotional, or social development, in comparison with normal expectations.
Muscle contractions (hypertonia) which can interfere with movement, speech, and walking and loss of ability to coordinate muscular movement (ataxia).
Uncontrolled movement of the eyes (nystagmus) and often reduced vision. Some people can have a squint in which one or both eyes turns inwards (esotropia).
Epilepsy, there are different forms of epilepsy e.g. absence episodes where the person may appear to be staring into space with or without jerking or twitching movements of the eye muscles, or more generalised tonic-clonic seizures, a type of generalised seizure that affects the entire brain. Tonic-clonic seizures are more commonly associated with epilepsy.
Although the majority of the signs and symptoms seen in people with MLD are brain related, some people may have inflammation of the gall bladder and can develop gallbladder polyps. All forms are progressive and regardless of the type, final stages of the disease is often characterised by blindness, inability to move with paralysis from the neck down, unresponsiveness, and an inability to speak.
Late infantile MLD
After a period of normal growth and development from birth, the most common initial signs and symptoms are movement related such as abnormal or erratic crawling or walking. Children learn to walk but may take longer than normal, over time this ability diminishes as muscles start to become rigid. Limb movement may become painful as contractures develop. The ability to write, draw or picking up items is also affected. Speech gradually becomes slower as the disease progresses. Mobility and speech are eventually lost and children become bedridden. There may be difficulties with feeding and weight gain and a feeding tube may become necessary.
Juvenile MLD
In the early stages children may have difficulties with movement and coordination such as clumsiness when walking. Children can develop slurred speech and their ability to concentrate is affected which may lead to behavioural problems at school. The situation may remain stable for months or even years, but as symptoms develop limb movement diminishes. Muscles become rigid and children eventually lose the ability to walk.
Adult MLD
Early signs and symptoms in adults who develop MLD may be reflected in poor performance at school or work and may be suggestive of a psychiatric disease, particularly schizophrenia. There is generally a slow decline in intellectual capabilities and people may become emotionally unstable and experience lapses in memory. Psychiatric symptoms such as hallucinations and delusions may develop. Movements may become clumsy and incontinence can become a problem. Paralysis of the arms and legs develop progressively. Loss of feeling and sensation may occur in the hand and feet (peripheral nerve damage) and seizures are rare.
Medication for controlling cough and cold symptoms and mucus production is available but it is essential to consult the doctor rather than using ‘over the counter’ medication which may not help. Medications such as antihistamines may dry out the mucus making it thicker and harder to dislodge. Decongestants usually contain stimulants that can raise blood pressure and narrow blood vessels. Cough medicines that have a sedating effect may cause more problems with sleep apnoea by depressing muscle tone and respiration.
Some medications for seizure control can also increase the secretions and the balance between seizure control and secretion control can be very hard to balance. Bacterial infections should be treated with antibiotics, but repeated use can also cause thrush, a fungal infection which commonly affects the mouth or vagina and produces a white curd-like deposit. It causes irritation and discomfort and will need to be treated.
Haematopoietic Stem Cell Transplantation (HSCT)
HSCT has been used to treat people with MLD. This procedure is not currently recommended for children with the late infantile form of MLD. HSCT may potentially be beneficial in people with late juvenile or adult onset MLD who are in the early stages of the disease.
For an up-to-date list of current UK based trials taking place visit Be Part of Research (resource provided by the National Institute for Health Research). For an international search visit Clinical Trials (resource provided by the U.S. National Library of Medicine).
This resource provides information on trial status including recruiting, completed or withdrawn and worldwide trial locations. To find out more about past or current trials speak to your doctor and learn about the risks and potential benefits.
The MPS Society is the only UK charity at the forefront of supporting people and families affected by MPS and related diseases. Our extensive support services offer you a wide range of support and resources.
The team can advise and sign post you to adequate needs-led support and services in your local area as well as social care, home adaptions, education and much more.
The support team can visit you in your home and provide you with vital support.
Get involved and support us in the community, volunteer or support fundraising; we are a small charity but with your support we can continue to offer a highly valued and essential service.
Need someone to talk to?
Our support includes an active listening service and telephone helpline.
Latest updates
My daughter Eva
For Leukodystrophy Awareness Month we hear from Catrin, whose daughter has Metachromatic Leukodystrophy (MLD). My daughter Eva Rae...
My son Joey
For Leukodystrophy Awareness Month we hear from Katie, whose son has Metachromatic Leukodystrophy (MLD). Joey was born a happy healthy...
Christine Lavery Memorial Fund opens a call for applications for summer vacation studentships 2023
The MPS Society are delighted to announce that we are launching the Christine Lavery Memorial Fund on 21 November, Christine’s birthday,...
Latest resources
BBC documentary highlights the importance of Newborn Screening for early diagnosis
BBC documentary highlights the importance of Newborn Screening for early diagnosis.
White paper on improved outcomes for children with MLD following gene therapy
Recently published white paper on the improved outcomes for children with MLD following gene therapy based on findings from a parent survey.
Be prepared: emergency information for admission to hospital
Emergency information for admission to hospital that you should have to hand.