This disease includes a spectrum of symptoms, people at the severe end are labelled ML II and less severely affected people are considered to have ML III. The prognosis is poor with a fatal outcome most often occurring in childhood. Most children with ML II may die before the age of 3 or 4 years old, some who are less severely affected have lived to the age of 10 or 12 years old.
Appearance
From birth babies have poor muscle tone and reduced growth with gradually worsening skeletal deformities that affect the spine, hands, hips and bones. A limited range of motion of shoulder joints is noted at birth. Features apparent soon after birth include a flat face, eye sockets are shallow which makes the eyes appear prominent, flattened nasal bridge, prominent mouth and enlarged gums are. Coarsening of facial features is progressive. Skin is often thickened and lacking elasticity. Occasionally, there may be more body hair than normal (hirsutism). The neck is short, cheeks are often rosy and the eyebrows may be bushy and meet in the middle. The hair on the head can gradually turn white. Children with ML II will be severely restricted in growth. The majority will stop growing by the age of 3 and are unlikely to be taller than about 90cms.
Brain
Intellectual ability is affected. Children are likely to be restricted in what they learn but some learn to talk, sing and do simple sums and some children use their hands to sign, thereby communicating their needs.
Heart
Heart murmurs can happen when heart valves become damaged by stored unwanted molecules. The heart valves are designed to keep blood flowing in the right direction. If a valve is weakened or changed in shape it may not work properly and a small amount of blood may leak in the wrong direction. Some children with ML II may develop problems with one of the heart valves but they may have valvular heart disease for years without any ill effects. If the condition worsens an operation may be possible to replace the damaged valves.
An electrocardiogram (ECG) test is used to identify problems with heart muscle, function and valves, it is a painless procedure and is often carried out annually (or as often as the doctor thinks necessary) to show whether any problems are starting.
Lungs
The movement of the lungs is restricted by the shape of the chest preventing the lungs to take in a large volume of air. There is an increase in secretions which are harder to clear as the restricted lungs make it difficult for people with ML II to take a deep enough breath to cough properly. When the lungs are not fully cleared there is an increased risk of infection which can lead to scarring of the airways causing further obstruction. Children with ML II are prone to frequent chest infections and tend to have runny noses.
Medication for controlling cough and cold symptoms and mucus production is available but it is essential to consult the doctor rather than using ‘over the counter’ medication which may not help. Medications such as antihistamines may dry out the mucus making it thicker and harder to dislodge. Decongestants usually contain stimulants that can raise blood pressure and narrow blood vessels, both are undesirable effects for people with ML II. Cough medicines that have a sedating effect may cause more problems with sleep apnoea by depressing muscle tone and respiration. It is common for children with ML II to develop secondary bacterial infections which should be treated with antibiotics.
Liver, Spleen and Abdomen
For children with ML II the liver and spleen become enlarged because they are storing mucopolysaccharides. The enlarged liver does not cause problems or lead to liver failure however the size can interfere with eating and breathing. The enlarged liver and spleen coupled with weakness of the tummy (abdominal) muscles can lead to a hernia. A hernia is when an organ, such as the intestine, pushes through a weak spot in the muscle that holds it in place. Treatment options differ depending on the type of hernia, in some cases surgery is needed.
Bones and joints
The spine bones (vertebrae) are poorly formed and may have a hump on the upper back called kyphosis and the neck region (cervical spine) may be fragile. Joint stiffness does lead to limited movement, in the shoulders and arms, hips and knees. The limited movement can make everyday activities like getting dressed difficult. Joint stiffness can sometimes cause pain which may be relieved by warmth and painkillers, speak with your doctor to select the most suitable treatment.
The shape of the hands of those affected ML II is very noticeable, they are short and broad, with stubby fingers which gradually become curved over or clawed. Normally joints are held in place by strong ligaments, children with ML II have loose or stretchy ligaments. As a child with ML II grows older the knees gradually become more knocked. It is sometimes possible for the legs to be straightened by an operation but it is best to wait until the child has stopped growing.
Ears
Some degree of deafness is common in people with ML II. It may be conductive deafness, nerve deafness or both (called mixed deafness) and can be made worse by frequent ear infections.
Conductive deafness is when sound waves that travel through the ear canal, drum and the middle ear are impaired. Correct functioning of the middle ear depends on the pressure behind the ear drum being the same as that in the outer ear canal and the atmosphere. This pressure is kept equal by the eustachian tube which runs from the middle ear to the back of the nose. If the eustachian tube is blocked the pressure behind the eardrum will drop and the transmission of sound waves will be impaired. If this persists, fluid from the lining of the middle ear will build up and in time will become thick like glue, hence the condition being known as glue ear. Glue ear can be treated through surgery by inserting a small ventilation tube called a grommet, however these can fall out quickly and T-tubes, a type of grommet which stays in place longer, are an alternative option.
Nerve deafness is damage to the tiny hair cells in the inner ear. It may happen at the same time as conductive deafness, in which case it is referred to as mixed deafness. Mixed deafness can be managed by grommets or hearing aids. Nerve deafness is managed by fitting hearing aids in most people. More severely affected children may keep pulling out their hearing aids at first, but it is important to persevere at wearing them so that communication can be maintained. Alternatives include radio aids and the loop system which can be helpful at school and at home.
Eyes
Clouding of the cornea caused by storage of waste products may be seen in children with ML II, however this rarely interferes with vision and is not particularly noticeable.
Dental
Good dental hygiene is very important for children with ML II, teeth should be well cared for to avoid tooth decay, pain and extractions. Usually teeth are widely spaced and poorly formed with fragile enamel. Cleaning around the mouth with a small sponge or a stick soaked in mouthwash will help keep the mouth fresh and avoid bad breath. If the water in your area has not been treated with fluoride, speak with your dentist about including fluoride tablets or drops as part of the dental management plan. Dribbling is a common problem and can soak through clothes causing soreness, to prevent this choosing a bib that is plastic backed.
Where a child with ML II is severely affected it may be safer for any treatment to be carried out in hospital. If teeth need to be removed under anaesthetic this should be carried out in hospital under the care of an experienced anaesthetist and never in the dental surgery. It is important to inform the dentist about heart problems when discussing any treatment. This is because certain bacteria in the mouth may get into the blood stream and cause an infection on the heart valves. In most cases antibiotics are usually prescribed before and after any dental treatment.
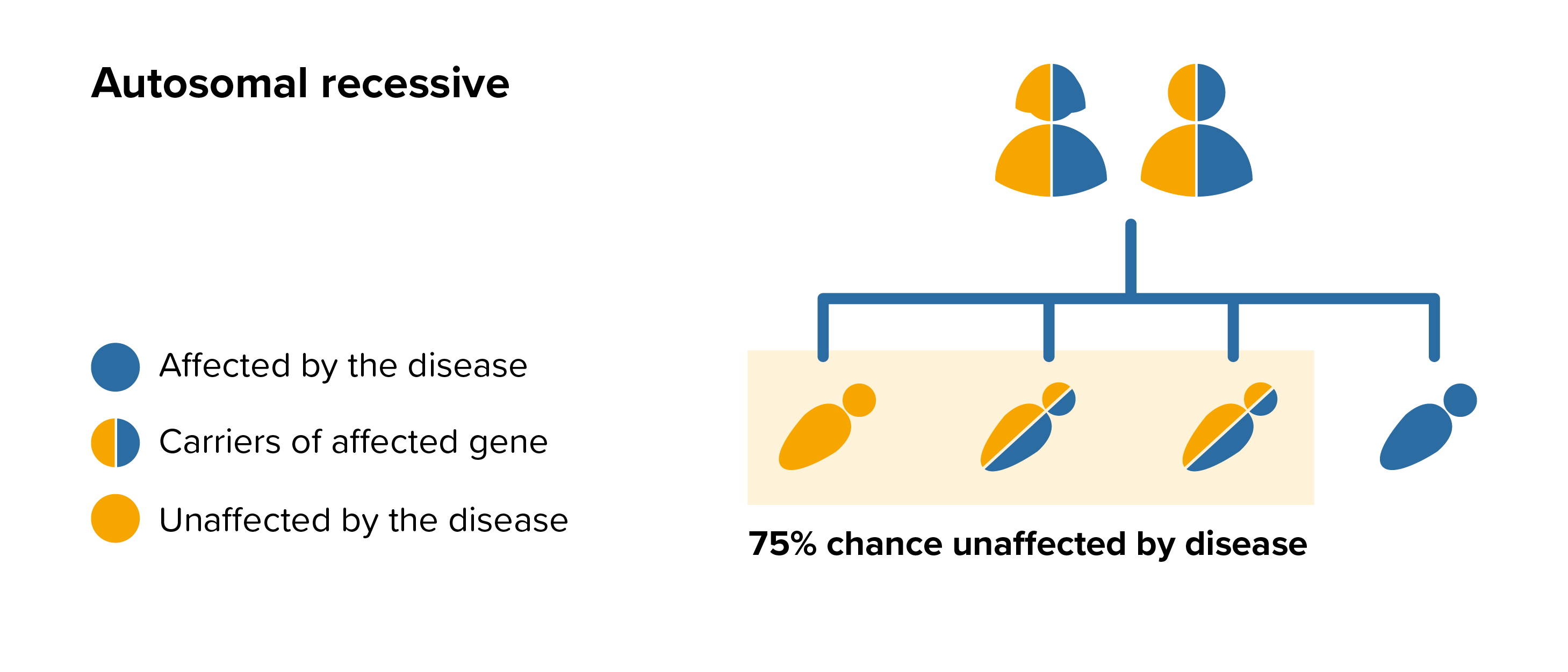 All parents of children with ML II can benefit from genetic counselling, the counsellor can provide advice on the risk to close relatives and to suggest whether the wider family should be informed. To find out during a pregnancy, if the baby is affected by ML II, screening tests can be arranged early on during a pregnancy for those families who already have a child with ML II. Where only one parent is a carrier, they can opt for carrier screening but it is not 100% reliable or accurate and is not possible in all cases.
All parents of children with ML II can benefit from genetic counselling, the counsellor can provide advice on the risk to close relatives and to suggest whether the wider family should be informed. To find out during a pregnancy, if the baby is affected by ML II, screening tests can be arranged early on during a pregnancy for those families who already have a child with ML II. Where only one parent is a carrier, they can opt for carrier screening but it is not 100% reliable or accurate and is not possible in all cases.