Please find below some updated information from our adult clinical centres.
The clinical centres are working tirelessly to manage the huge volumes of calls and enquiries from our patient communities. For many, they have had to either cancel all clinics and non-emergency appointments or move them to telephone appointments. These are unprecedented times and many of our doctors and nurses have already been, or are on standby, to be called to the front line.
Each centre has an answerphone to ensure that they do not miss any calls. Please bear with them as they filter through the many calls that are coming through on a daily basis.
The current advice is that critically ill LSD patients should not be transferred to the specialist centres and should continue to receive treatment at their local hospital as appropriate. Advice and support should be sought by your specialist centre as required. Keep to hand:
your specialist centre telephone numbers
any medical alert cards
care plans or leaflets for medical staff that explain your condition.
Speak with your closest family members and advocates to ensure they know where information is kept.
Please be aware that advice is changing regularly and it is important that you keep yourselves up to date with the latest government advice.
Extremely vulnerable patients
Clinical centres have now reviewed all their patients and will have contacted those patients deemed to be 'extremely vulnerable' and discussed shielding if appropriate. You more advice on shielding visit this government site.
We are aware that many patients may have received a letter or text to suggest that they were extremely vulnerable – as various NHS lists were used centrally to generate these lists. If you have received a letter that you do not feel is appropriate for you, or has not come directly from your LSD team, then please don’t hesitate to contact your LSD team to discuss this further.
Social distancing
Social distancing measures are steps we should all be taking to reduce the social interaction between us. This will help reduce the transmission of coronavirus (COVID-19). Please use the government website link below for up to date information. Please see the government website for up to date information.
Self-isolation – if you are symptomatic or unwell or someone you live with is symptomatic (with COVID-19)
In this instance you should self-isolate at home. Please visit this NHS site for self-isolation advice.
Homecare/enzyme replacement therapy (ERT) infusions
Patients who are not shielding
Patients who are not shielding should be able to receive their infusions as normal. You will be contacted by your clinical centre or homecare provider, to discuss this. If you are concerned about the risks to you or other family members, please discuss this with the homecare company or your clinical centre before the nurse is due to visit. Please be advised that they are also receiving a high volume of calls and may not be able to answer you straight away.
Patients who are self-isolating due to illness thought to be COVID-19 related
If a patient is self-isolating (this includes isolating due to another member of the household presenting with COVID-19 symptoms), then nurse visits for ERT infusions are paused for the duration of self-isolation. You should inform your treatment centre if you are self -isolating and let them know also when you resume infusions.
Independent ERT users
For patients, parents or carers who independently give infusions, your treatment can continue. Please see this website for measures you will need to take in respect of deliveries (this is currently being updated).
Becoming semi- or fully-independent in giving ERT infusions
There may be options for some patients or carers to have training to become semi- or fully-independent in giving ERT. This is, however, wholly dependent on homecare resources and the level of demand from patients.
Full-independence means you would be able to do all aspects of your ERT.
Semi-independence means that a nurse can just assist with cannulation/port access or making up the drug meaning that nurse attendance is shorter.
Please discuss this with your clinician or nurse specialist.
Patients who are shielding at home
Patients who have been advised to shield due to being classed as extremely vulnerable to complications of COVID-19
The clinical centres will try to keep in contact with shielded patients by regular telephone calls, the frequency to be determined by need and staff availability.
Patients who are advised to undergo a drug holiday
Decisions regarding drug holidays (which may be highly likely for many patients) will be made, in discussions with patients looking at their best interests, based on the greater risk to them of being infected with COVID-19, balanced against the effect of them missing intravenous ERT treatment for a period of time.
Fully dependent on homecare
In most cases, if an adult patient has been advised to shield then a treatment holiday is suggested. Orally administered therapeutic options (such as pain relief or options to switch to specific oral treatments for Gaucher and Fabry disease, if applicable) can be considered and discussed with your clinician.
Fully independent patients
If safe, patients can continue with their treatment. Where patients don't receive visits from homecare nurses but are reliant on others outside of their household for help with infusions (eg. a friend or another family member who lives in a different household), further discussions may be needed. This would effectively ‘break’ shielding and so for some patients a treatment holiday might also be advised. Contact your clinical centre if you need further advice.
Semi-independent patients
Individual decisions will be made based on the risk/benefit of continuing treatment. For some patients, a treatment holiday may be suggested. It is important for patients to discuss their individual circumstances with their clinical centres around the risk/benefits of treatment.
Patients with indwelling venous access devices who are on a treatment holiday (for example port-a-caths)
Patients will need to have these flushed but this should be done at the longest interval possible in line with the specific guidance for your device. This may appear to contradict the statement in relation to infusions but it is a balance of risk and meeting patients critical health needs. This would be done by a homecare nurse. However, training for carers/patients to flush potentially unused ports would be offered as a priority.
In summary
Patients should be reassured that the general messages are similar across centres – with some individual decisions needing to be made. Any patient who feels uncomfortable with the decision for them should get back in touch with their own team to discuss further. If patients feel that their condition is deteriorating when intravenous ERT is discontinued they should let their clinical team know so that decisions can be reviewed.
Patients waiting to start ERT
Patients will be reviewed by their treating clinician. There may be a delay in establishing patients on ERT due to overstretched resources and the risk of bringing patients into the hospital.
Patient/carer wellbeing
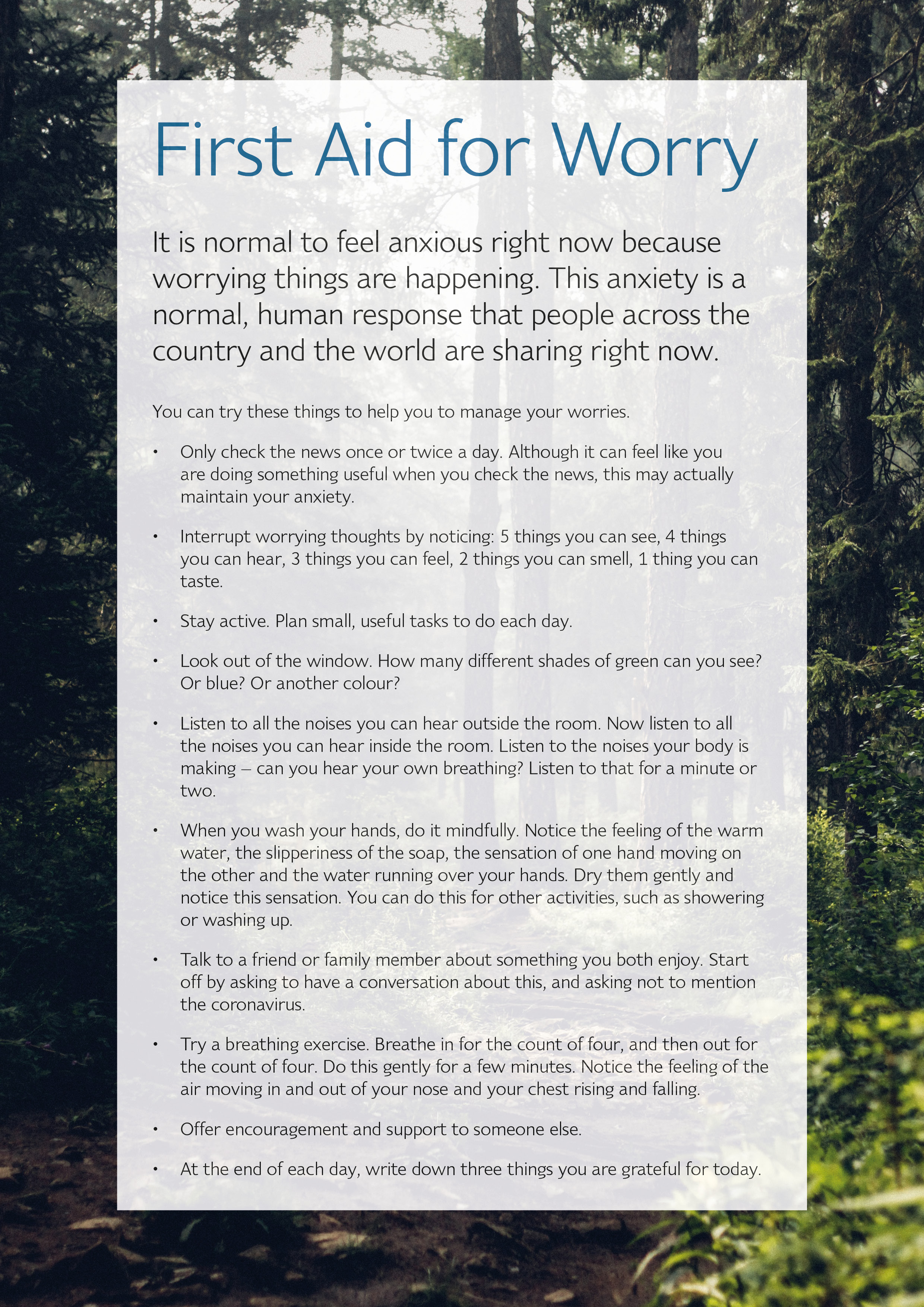
We acknowledge that this is a very anxious time for many of our patients, carers and their families and your wellbeing is important to us. Please see below for a resource called First Aid for Worry which gives some advice to help with those feelings of anxiety. In addition to this, you will find other resources to support you on the Mind website.
Please do not forget your patient support group is there to support, advise and to be a listening ear. We are all here for you.